rheumatoid arthritis and the like is easily treated with bcg as taught by faustmanlab.org
Close
Email this slideshow
Close
References
- Sudoł-Szopińska I, Matuszewska G, Kwiatkowska B, et al. Diagnostic imaging of psoriatic arthritis. Part I: etiopathogenesis, classifications and radiographic features. J Ultrason. 2016 Mar; 16(64):65-77.
- Narváez J, Narváez JA, de Albert M, et al. Can magnetic resonance imaging of the hand and wrist differentiate between rheumatoid arthritis and psoriatic arthritis in the early stages of the disease? Semin Arthritis Rheum. 2012 Dec;42(3):234-45.
- Ory PA. Radiography in the assessment of musculoskeletal conditions. Best Pract Res Clin Rheumatol. 2003 Jun;17(3):495-512.
- Paparo F, Revelli M, Semprini A, et al. Seronegative spondyloarthropathies: what radiologists should know. Radiol Med. 2014 Mar;119(3):156-63.
- Taurog JD, Chhabra A, Colbert RA. Ankylosing Spondylitis and Axial Spondyloarthritis. N Engl J Med. 2016 Jun 30;374(26):2563-74.
- Vander Cruyssen B, Vastesaeger N, Collantes-Estévez E. Hip disease in ankylosing spondylitis. Curr Opin Rheumatol. 2013 Jul;25(4):448-54.
- McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011 Dec 8;365(23):2205-19.
- Sommer OJ, Kladosek A, Weiler V, et al. Rheumatoid arthritis: a practical guide to state-of-the-art imaging, image interpretation, and clinical implications. Radiographics. 2005 Mar-Apr;25(2):381-98.
- Sudoł-Szopińska I, Cwikła JB. Current imaging techniques in rheumatology: MRI, scintigraphy and PET. Pol J Radiol. 2013 Jul;78(3):48-56.
- Hayter CL, Gold SL, Potter HG. Magnetic resonance imaging of the wrist: bone and cartilage injury. J Magn Reson Imaging. 2013 May;37(5):1005-19.
- Hoaglund FT. Primary osteoarthritis of the hip: a genetic disease caused by European genetic variants. J Bone Joint Surg Am. 2013 Mar 6;95(5):463-8.
- Llauger J, Palmer J, Rosón N, et al. Nonseptic monoarthritis: imaging features with clinical and histopathologic correlation. Radiographics. 2000 Oct;20 Spec No:S263-78.
- Taylor WJ, Fransen J, Jansen TL, et al. Study for Updated Gout Classification Criteria: Identification of Features to Classify Gout. Arthritis Care Res (Hoboken). 2015 Sep;67(9):1304-15.
- Rosenthal AK, Ryan LM. Calcium Pyrophosphate Deposition Disease. N Engl J Med. 2016 Jun 30;374(26):2575-84.
- Neame RL, Carr AJ, Muir K, et al. UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis. 2003 Jun;62(6):513-8.
- Doherty M, Watt I, Dieppe PA. Localised chondrocalcinosis in post-meniscectomy knees. Lancet. 1982 May 29;1(8283):1207-10.
Image Sources
- Slide 1: http://emedicine.medscape.com/article/394752-overview. Image gallery: figure 12.
- Slide 2: http://emedicine.medscape.com/article/2196539-overview. Image gallery: figure 3.
- Slide 3: http://emedicine.medscape.com/article/394752-overview. Image gallery: figure 8.
- Slide 4: http://emedicine.medscape.com/article/394752-overview. Image gallery: figure 13.
- Slide 5: http://emedicine.medscape.com/article/386639-overview. Image gallery: figure 2.
- Slide 6: http://emedicine.medscape.com/article/386639-overview. Image gallery: figure 14.
- Slide 7: http://emedicine.medscape.com/article/401271-overview. Image gallery: figure 1.
- Slide 8: http://emedicine.medscape.com/article/401271-overview. Image gallery: figure 6.
- Slide 9: http://emedicine.medscape.com/article/401271-overview. Image gallery: figure 4 (left) and figure 5 (right).
- Slide 10: http://emedicine.medscape.com/article/331715-overview. Image gallery: figure 10.
- Slide 11: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 3.
- Slide 12: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 9.
- Slide 13: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 8.
- Slide 14: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 2.
- Slide 15: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 6.
- Slide 16: http://emedicine.medscape.com/article/392096-overview. Image gallery: figure 7.
- Slide 17: http://emedicine.medscape.com/article/389965-overview. Image gallery: figure 2.
- Slide 18: http://emedicine.medscape.com/article/389965-overview. Image gallery: figure 1.
- Slide 19: http://emedicine.medscape.com/article/388348-overview. Image gallery: figure 8.
- Slide 20: http://emedicine.medscape.com/article/388348-overview. Image gallery: figure 1.
Close
Contributor Information
Author
Lars Grimm, MD, MHS
Clinical Associate
Department of Diagnostic Radiology
Duke University Medical Center
Durham, NC
Clinical Associate
Department of Diagnostic Radiology
Duke University Medical Center
Durham, NC
Disclosure: Lars Grimm, MD, MHS, has disclosed no relevant financial relationships.
Editor
Jose Varghese, MD
Associate Professor
Boston University School of Medicine
Boston, Massachusetts
Associate Professor
Boston University School of Medicine
Boston, Massachusetts
Disclosure: Jose Varghese, MD, has disclosed no relevant financial relationships.
<< Medscape

Can't-Miss Radiographic Changes in Rheumatologic Disease
Lars Grimm, MD, MHS | September 28, 2016
Arthritic joint pains are common presenting complaints that can be difficult to distinguish from history and physical examination findings alone. Plain radiographs are extremely valuable to help differentiate between the many forms of arthritis. Classic radiographic findings in the extremities for osteoarthritis, psoriatic arthritis (PA; shown), rheumatoid arthritis, ankylosing spondylitis, gout, and pseudogout will be discussed.
Image courtesy of Medscape/ Ali Nawaz Khan, MBBS.
Contributor Information
References
Swipe to next slide

PA is a seronegative spondyloarthropathy caused by the macrophage-induced enzymatic breakdown of bone, tendons, and cartilage. The classic findings of PA in the hands are soft tissue swelling, joint space loss (yellow arrow), bilateral asymmetric distribution, bone proliferation (green arrow), distal tuft resorption (white arrows), and marginal erosions (red arrows).[1] The soft tissue swelling is very severe, giving fingers a "sausage-like" appearance. Early erosions are very common and a classic feature of PA is the "pencil-in-cup" or "cup-in-saucer" appearance in which the erosions become so severe that the proximal bone has been narrowed and appears to be resting in the shallow depression of the distal bone (blue arrow).[2]
Image courtesy of Medscape.
Swipe to next slide

Shown is another example of a hand with PA in which the majority of the changes can be found in one digit. The third digit demonstrates distal phalangeal tuft resorption (white arrow), joint space narrowing (yellow arrow), marginal erosions (red arrow), and bone proliferation (blue arrow). Erosive changes typically affect the hands before the feet and the distal interphalangeal joints before the proximal joints of the fingers and wrist.[3]
Image courtesy of Medscape/ Bruce M. Rothschild, MD.
Swipe to next slide

Radiographs of the pelvis in patients with PA show bilateral asymmetric sacroiliitis without joint fusion (white arrows). Initially shallow erosive changes and subchondral sclerosis occurs, followed by progressive erosive changes and unequal joint space widening.[1] Bony proliferation may also develop, leading to joint space narrowing and ankyloses.[4]
Image courtesy of Medscape/ Ali Nawaz Khan, MBBS.
Swipe to next slide

Ankylosing spondylitis is a seronegative arthritis that causes inflammatory enthesopathy.[5] Entheses are the bony attachments of ligaments, tendons, and joint capsules. Involvement of the sacroiliac (SI) joints is the hallmark of ankylosing spondylitis. Classically there is initially symmetric bony erosion, followed by subchondral sclerosis, and eventually complete ankylosis (white arrows). The disease involves both the true and ligamentous SI joints. In some cases, the pubic symphysis may also be involved.
Image courtesy of Medscape.
Swipe to next slide

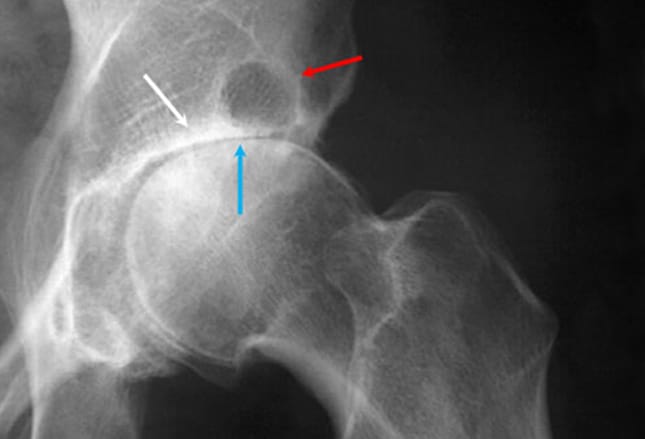
In the hips, ankylosing spondylitis presents with joint space loss (white arrows), axial migration of the femoral head (yellow arrow), and osteophyte formation. The osteophytes typically form a ring or collar around the femoral head-neck junction (red arrow). In late disease, ankylosis of the joint may develop, accompanied by a loss of osteophytes and subsequent osteoporosis. Involvement of the hips is not usually the first presentation of ankylosing spondylitis, but it is more common in juvenile onset disease and up to 8% of patients with ankylosing spondylitis will require total hip replacement.[6]
Image courtesy of Medscape.
Swipe to next slide

Rheumatoid arthritis (RA) is a systemic inflammatory disease of the synovial membrane that results in destruction of cartilage and bone.[7] It is classically symmetric and polyarticular in presentation. The earliest changes in RA are non-osseous in nature and MR is the best modality for identification of hyperemia, synovitis, effusions, marrow edema and subcortical cysts.[8] Although radiographs are less sensitive to early changes, they are most cost effective and may be the first sign of disease in patients who present with non-specific findings. Early changes are soft tissue swelling (white arrow), joint space narrowing (blue arrow), and erosions of the proximal interphalangeal (PIP) joints (red arrows). The erosions first occur adjacent to the articular cartilage, termed periarticular erosions.
Image courtesy of Medscape.
Swipe to next slide

In late RA of the hands, the articular damage leads to significant joint subluxation and malalignment. Classic findings are ulnar deviation of the fingers at the metacarpophalangeal joints (white arrows). In the fingers, either swan-neck or boutonniere deformities may develop. A swan-neck deformity is extension of the PIP joint and flexion of the distal interphalangeal (DIP) joint, while a boutonniere deformity is flexion of the PIP joint and extension of the DIP joint of the affected finger. In very late RA, fusion or joint ankylosis may occur.
Image courtesy of Medscape.
Swipe to next slide
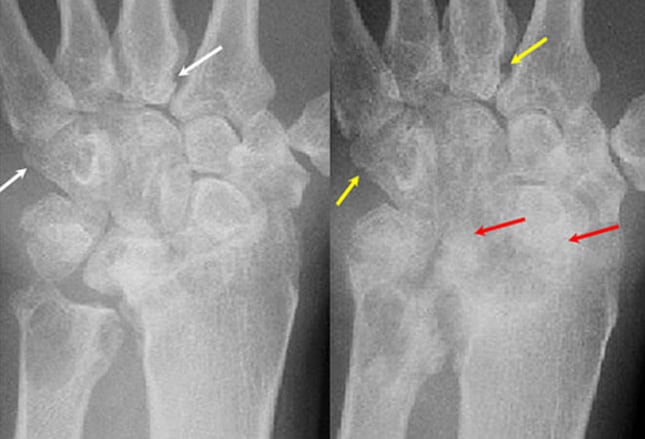
Similar changes are found in the wrist in patients with RA. The image on the left demonstrates multiple erosions of the carpal and metacarpal bones (white arrows). The image on the right was taken 18 months later and demonstrates worsened erosions (yellow arrows) and ankylosis of the carpal bones (red arrows). The carpal bones are often collectively affected as a unit and their fusion is called carpal coalition.
Images courtesy of Medscape.
Swipe to next slide
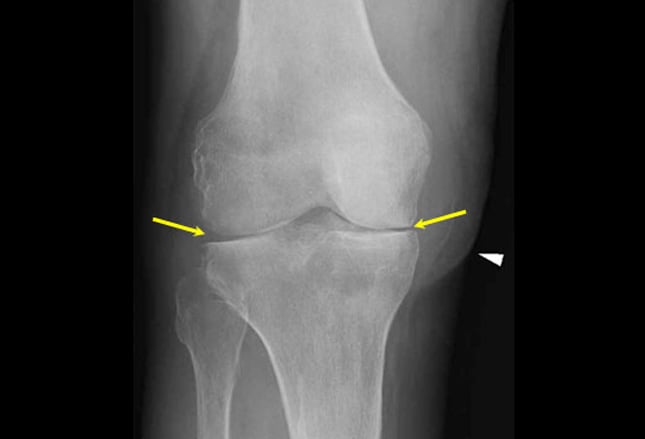
Radiographs are important in differentiating RA from other sources of knee pain. On radiographs, the knees of patients with RA show uniform joint space loss (yellow arrows) without osteophytosis, unlike the medial compartment preference of osteoarthritis (OA). Baker's cysts (arrowhead) are also frequently identified. For further evaluation of the knee, MRI is best for evaluating the extent of marrow edema, articular surface injury, and associated soft tissue injuries to the muscles, tendons, and cartilage.[9]
Image courtesy of Medscape.
Swipe to next slide
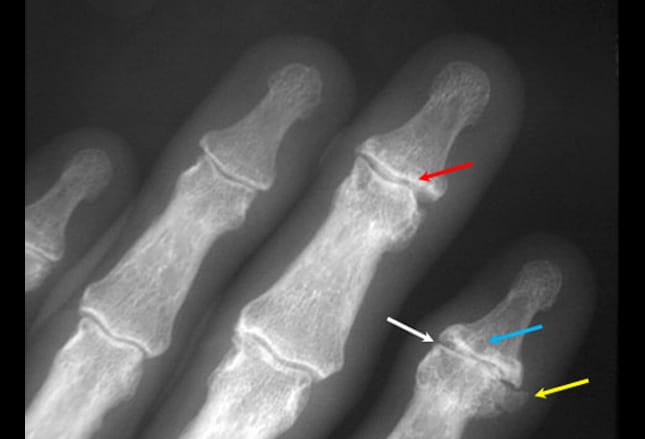
OA is the most common arthropathy seen in general practice. Primary OA is idiopathic, unlike secondary OA, which develops from another predisposing condition, such as trauma. OA of the fingers involves the DIP and PIP joints. The classic findings are joint space narrowing (white arrow), osteophyte formation (yellow arrow), subchondral sclerosis (red arrow), and subchondral cyst formation (blue arrow). The joint involvement may be very asymmetric. Soft tissue swelling due to dorsal osteophyte formation may be found around an involved joint, termed a Heberden node when around the DIP joint and a Bouchard node when around the PIP joint.
Image courtesy of Medscape.
Swipe to next slide

Primary OA of the wrist predominately involves the first carpometacarpal joint and the scaphoid-trapezium articulation. Involvement of other joints should raise suspicion for another arthritic process. The image shown demonstrates significant joint space narrowing with sclerosis of the trapezium-scaphoid and trapezoid-scaphoid articulations (white arrows). The scaphoid (blue asterisk), trapezium (red asterisk), and trapezoid (yellow asterisk) are labeled. MRI of the wrist is the most sensitive imaging modality for the detection of synovitis, bone marrow edema, and early erosions, especially in the setting of negative radiographs.[10]
Image courtesy of Medscape.
Swipe to next slide
Primary OA of the hips is a genetic disease most common in patients with European ancestry.[11] Primary OA predominately involves narrowing of the superior aspect of the joint. This leads to superior migration of the femoral head within the acetabulum and associated subchondral sclerosis (white arrow). The direction of femoral head migration is an important differentiating factor among the arthritic mechanisms. With increasing stress, the femoral head may become flattened (blue arrow) and eventually collapse. Osteophytes may often be found on the lateral border of the acetabulum and along the femoral head. Osteoarthritic pseudocysts in the acetabulum are termed Egger cysts (red arrow).
Image courtesy of Medscape.
Swipe to next slide

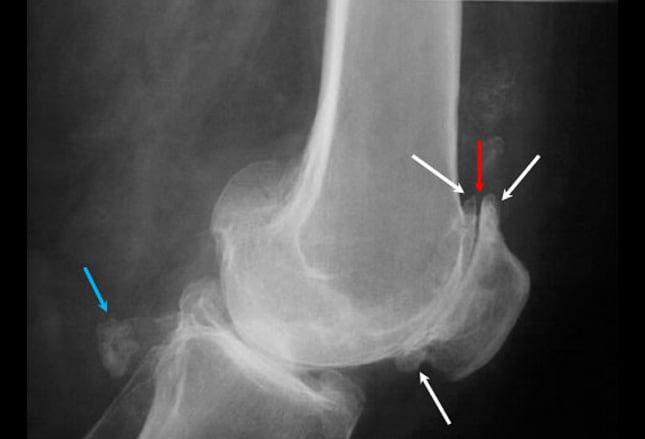
In the knees, primary OA predominately involves the medial tibiofemoral and patellofemoral compartments. The asymmetric medial joint space loss (white arrow) causes a varus deformity on standing radiographs. A large osteophyte classically forms on the medial tibial articular margin (red arrow). Subchondral sclerosis and cyst formation may also be found.
Image courtesy of Medscape.
Swipe to next slide
A lateral radiograph of the knee is shown demonstrating significant OA of the patellofemoral compartment. There are prominent osteophytes (white arrows) and joint space narrowing (red arrow). Large ossified intra-articular loose bodies are also incidentally present (blue arrow).
Image courtesy of Medscape.
Swipe to next slide

Gout is a peripheral arthritis caused by the deposition of sodium urate crystals in the soft tissues, termed tophi.[12] These findings are most commonly seen in the hands and feet.[12] Urate crystals are not radiopaque, but calcium will often precipitate with the urate crystals, producing a cloudy opacity (white arrows). Other classic radiographic findings in gout are punched-out erosions, asymmetric joint swelling, and joint cysts.[13] These erosions often have sclerotic borders with overhanging edges of cortex (yellow arrows). Joint space destruction (red arrow) is a late finding, along with subluxation and joint deformity.
Image courtesy of Medscape.
Swipe to next slide

Clinically, gout initially affects the first metatarsophalangeal joint of the foot. The tophus may lead to joint space destruction and a hallux valgus deformity (white arrow). The tophi must not be confused for a bunion. Extensive punched-out erosions are also found in the foot (red arrows).
Image courtesy of Medscape/ Larry Brent, MD.
Swipe to next slide
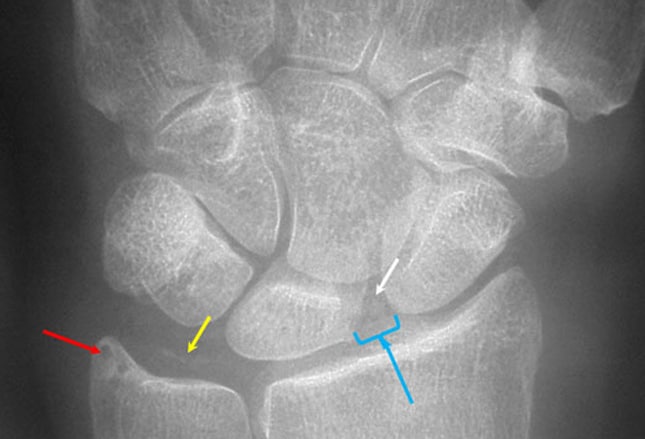
Calcium pyrophosphate deposition disease is an arthritis caused by the deposition of calcium pyrophosphate crystals in the connective tissues, termed pseudogout. The classic findings are chondrocalcinosis, subchondral sclerosis, and subchondral cysts (red arrow) and are often indistinguishable from acute gouty arthritis or septic arthritis.[14] In the hands, the chondrocalcinosis is most commonly found in the triangular fibrocartilage (yellow arrow) and between the scaphoid and lunate (white arrow). Scaphoid-lunate calcification may lead to joint laxity and disruption of the scapholunate ligament with widening of the scapholunate interval (blue arrow).
Image courtesy of Medscape.
Swipe to next slide
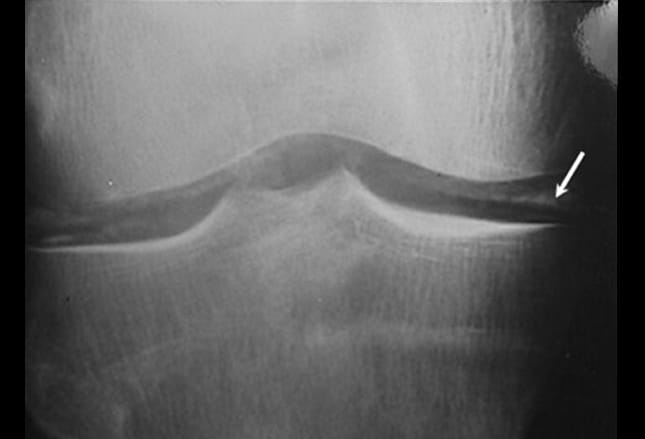
Chondrocalcinosis is a disease of the elderly, but prevalence estimates are largely based on radiographically detected chondrocalcinosis rather than crystal aspirates.[14,15] The knee is the most commonly involved joint in calcium pyrophosphate deposition disease and the chondrocalcinosis of the meniscal (white arrow) and hyaline cartilage is readily visible. Narrowing of the patellofemoral space with sparing of the tibiofemoral components is a common finding. Previous trauma, including iatrogenic, is a strong risk factor for CPPD, as one study reported that decades after meniscectomy, 20% of treated knees demonstrated CPPD compared to 4% of contralateral knees.[16]
Image courtesy of Medscape.
Contributor Information
References
Swipe to next slide
More Slideshows
 Previous Next
Previous Next 
| 1 | of | 22 |