Facing Down the World's Deadliest Pathogens in a BSL4 Lab
Researchers reach a crucial milestone despite the challenges of working under astronaut-like conditions
- By Bob Roehr on
Ebola, smallpox, plague—the rogue’s gallery of highly infectious deadly pathogens is frighteningly long and their potential for havoc is great, which is why they can only be studied within the tightly controlled confines of a biosafety level 4 (BSL4) facility. The precautions make work in a BSL4 extremely demanding, slow and physically taxing, which is one reason such research lags behind studies of less-lethal organisms.
An Australian research team, however, recently reached a milestone when it became the first to screen and catalogue all of the genes activated by a BSL4 pathogen when it infects human cells. Their focus was the obscure but deadly Hendra virus, which causes respiratory disease in horses and can cross over into humans; they recently published their findings in PLoS Pathogens.
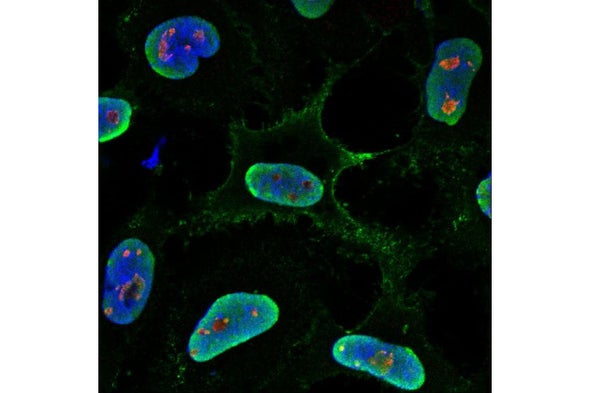
The researchers used siRNA—small bits of synthetic RNA employed to silence an individual gene—in cells placed in the well of a microarray plate, then exposed the cells to the virus and examined where the Hendra thrived and where it died. Little or no virus in a well meant that the siRNA-suppressed gene was important for viral replication, explains molecular biologist Cameron Stewart, who led the effort at the Commonwealth Scientific and Industrial Research Organization (CSIRO), Australia’s national science agency.
_door.jpg)
Credit: NIAID
The approach was simple but the scale was enormous, as there were multiple wells for quality control and the process was repeated for each of the approximately 20,000 human genes. It would have been difficult in a regular lab, but took years of work in the physically challenging setting of a BSL4.
“Several hundred proteins are involved to cause infection, but the one with the largest impact was a protein called fibrillarin,” Stewart says. “If you reduce the catalytic activity of fibrillarin you can block Hendra virus infection.” That was surprising, he explains, because “fibrillarin resides deep within the nucleolus of the host cell…[where it] methylates ribosomal RNA molecules, which then go on to form ribosomes,” but its full function may not be completely understood.
Silencing the gene that produces fibrillarin also stopped Nipah virus from replicating. Nipah is another henipavirus, a close cousin to Hendra with a high mortality rate in bats and humans in a zone stretching from Australia to Bangladesh. In fact, fibrillarin’s function appears to be similar across the entire paramyxovirus family, which includes measles and mumps, so perhaps understanding fibrillarin as a target for intervention and designing the right treatment for it could work against a broad range of viruses.
BSL4 FACILITIES
The continued emergence of deadly infections such as Ebola, MERS and SARS, as well as the terrorist use of anthrax in 2001—when spore-laced letters sent to elected officials in Washington and the news media killed five people and sickened 17 others—made government leaders aware of the need for more and better BSL capacity, and they have since provided substantial, sustained funding to support such facilities. Still, only a few dozen labs in the world are certified as BSL4 facilities; some are very small and only work on diagnostics, or cell cultures, or a single species of animals.
Most descriptions of a BSL4 facility focus on the physical aspects: elaborate negative-flow air filtration systems, airlocks to enter the “hot” space containing the pathogens, “space suits” with their own air supply systems, and rigorous decontamination procedures when exiting. In some ways it is as arduous as exploring the polar regions or outer space.
As are the demands placed upon the men and women who work every day in the bulky suits and restricted environment.
“Very quickly you learn not to have a coffee or go in feeling hungry,” says Glenn Marsh, the molecular biologist who did much of the physical work inside the Australian BSL4. “The negative airflow through the suit dehydrates you fairly quickly, so we try to be no more than about three hours at a time in a suit. It is very tiring.”
“There is nothing worse than being in the suit and having a runny nose,” says Lisa Hensley, deputy director of NIH’s Integrated Research Facility at Fort Detrick, Maryland. “You can’t blow your nose, so people got very creative with towels around their neck so they could blot their nose. And what do you do if you sneeze? You can’t clean your face shield.” That’s why they urge researchers to use judgment about when to “suit up.”

Sign up for Scientific American’s free newsletters.
Equipment failure is another challenge.“On more than one occasion Glenn would call me up and say, ‘The robotics are broken. We can’t fix it.’ We just had to turn everything off. The equipment had to be removed from the BSL4 lab, and it had to be decontaminated before it could be fixed,” Stewart recalls. And the cells that had taken two weeks to develop had to be discarded. It added even more time to the multi-year Australian project.
Hensley says the Fort Detrick lab was designed to minimize some of these issues. It is one of the largest BSL4 labs in the world, and one of the few built to include imaging capacity for animals using CT scans and MRIs. That equipment requires a lot of maintenance, so the facility was creatively designed with much of the machinery in a “cool” portion of the lab, where normal precautions are sufficient, and a tube running in from the strictly controlled “hot” part of the lab; the research animal is placed on a moving bed in the tube for imaging.
Another way researchers have sought to reduce time in a BSL4 facility is by constructing a pseudotype virus, a chimera that artificially combines elements from two different viruses which can be studied under less-restrictive conditions. Boston University microbiologist John Connor has done this with Ebola. He says he combined glycoproteins from the outer shell of the virus, which “unlocks a pathway for the virus to get into the cell,” with core functional genes from the vesicular stomatitis virus,which poses little risk to humans. This allows him to work in a lower-level BSL2 facility. Connor says the approach can work with some stages of the viral life cycle but not with others, and experiments on a pseudotype will always have to be confirmed using the actual virus; sometimes the two organisms behave differently.
The ultimate goal of BSL4 research is not simply to generate knowledge, but to advance toward prevention and treatment of deadly diseases. Stewart says his team’s initial work has not only identified fibrillarin as essential for viable paramyxovirus replication—it also has shown that one can “deplete fibrillarin from cells or block its catalytic activity and the vast majority of cellular proteins still get made within the cell,” which suggests it is a safe target for intervention. He hopes they can develop an antiviral drug that will be effective against the entire family of paramyxovirus.
No comments:
Post a Comment