do not let the united states take your life for its own lack of common sense experimentation
hospitals such as south nassau communities hospital in oceanside sbuse antibiotics such as vancomycin and fail to provide penicillin to patients
by altering gut bacteria by overuse misusue non selective use of antibiotics many lives are put at increased ridk of impairment or worse
eat shit if you are sick. there may be something to gain and little to loose
communicate with the parkinsons society
in memory of barbara rock who pushed me out into the lake in a styrofoam boat and said sail
no money for you michael j fox
we can do it ourselves better by reading and learning from clostridium
Questions? Want to donate by phone?
Call: 1-800-708-7644
Call: 1-800-708-7644
Or donate by mail:
Donation Processing
The Michael J. Fox Foundation
P.O. Box 5014
Hagerstown, MD 21741-5014
Donation Processing
The Michael J. Fox Foundation
P.O. Box 5014
Hagerstown, MD 21741-5014
eat feces snd observe wheher or not your parkinsons condition changes
Parkinson’s linked to gut bacteria
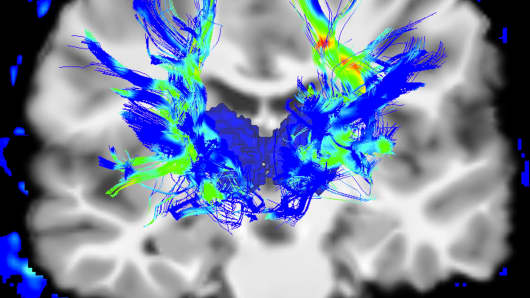
For the first time, researchers have found a functional link between the bacteria in the gut and the onset of Parkinson’s disease, one of the world’s most common debilitating brain disorders.
A team of scientists from several institutions in the United States and Europe showed how changing the bacteria in the guts of mice affected the manifestation of Parkinson’s symptoms — even including bacteria taken from the guts of humans with the disease.
The findings suggest a new way of treating the disease: The best target for treatment may be the gut, rather than the brain. The researchers hope the new information can be used to develop “next generation” probiotics, more sophisticated than the sort of probiotics found on the shelves of health food stores today.
“One can imagine one day, maybe in our lifetimes, patients will be prescribed drugs, and in the pills will be the bacteria that protect them from disease or even maybe treat their disease symptoms,” said Sarkis Mazmanian, one of the researchers on the team and professor of microbiology at the California Institute of Technology.
The scientists published their findings Thursday in the journal Cell.
More from Modern Medicine:
Why microbiome science is booming
Chinese first to test CRISPR gene editing in humans
A new drug is slowing memory loss in Alzheimer’s patients
Why microbiome science is booming
Chinese first to test CRISPR gene editing in humans
A new drug is slowing memory loss in Alzheimer’s patients
Parkinson’s disease is a neurodegenerative disorder where brain cells accumulate excessive amounts of a protein called alpha-synuclein and then die off. Patients lose motor function, experience tremors and shaking, and suffer other physical and mental effects. One million people in the U.S. and up to 10 million worldwide suffer from the condition. It is considered the world’s second most common neurodegenerative disease after Alzheimer’s.
It rarely runs in families; instead it appears to be influenced by environmental factors.
Previous research has suggested connections between gut bacteria and Parkinson’s, as well as other diseases such as multiple sclerosis. But no research has shown exactly how the two might be related.
The researchers performed three different experiments that showed the link between the germs in the gut and the disease in the brain.
First, the team acquired two sets of mice that had been genetically modified to overproduce alpha-synuclein — the protein that is the hallmark of the disease. One set of mice had a complete microbiome — the collective name for the bacteria in the gastrointestinal tract. The other set had no bacteria in their guts — they were germ-free.
The germ-free mice were still overproducing alpha-synuclein, but their brain cells were not accumulating the protein. The germ-free mice showed fewer symptoms and performed better on a series of motor skills tests meant to model the kinds of tests given to human patients.
However, the mice with the complete microbiome did begin accumulating the protein in their brain cells, and began showing brain damage in the regions that one would expect for a Parkinson’s patient.
Next the team fed both types of mice certain short-chain fatty acids that are commonly produced by bacteria in the gut. In other words, they were looking to see if even germ-free mice would show symptoms if the researchers mimicked gut bacteria activity.
And this time, the germ-free mice did show symptoms of the disease in the brain when fed the chemicals.
This suggested that the chemicals certain types of gut bacteria produce worsen conditions in the brain.
Finally, the team did a third experiment where they took samples of gut bacteria from human Parkinson’s patients and from healthy human controls and transplanted them into the germ-free mice that overexpressed alpha-synuclein. Remarkably, the mice began to exhibit symptoms. However, only the bacteria from the Parkinson’s patients caused symptoms in the mice. The germ-free mice given samples from healthy humans did not produce symptoms
In some ways, Mazmanian finds the third experiment most telling.
“At first pass, what this tells you is that it is not the presence or absence of bacteria that matters, it is the types of bacteria that are there,” he said.
In other words, it could mean that the guts of Parkinson’s patients have certain bacteria that contribute to the disease, or that they lack certain beneficial bacteria that could help protect against the disease.
Samples of gut bacteria in Parkinson’s patients render this possible. They tend to have certain kinds of bacteria not found in healthy people, and they also lack others that are found in healthy people, Mazmanian noted.
Moving forward, Mazmanian said the team would like to identify specific bacteria that are helpful of harmful and understand how they might contribute to or prevent the disease, and what kinds of treatments might produce the microbiome that best protects against the disease.
No comments:
Post a Comment